Mechanical Evaluation of Suture Anchors for Soft Tissue Repair
In this article, Element expert Maciej Jakucki reveals essential FDA testing methods for suture anchors - implants critical for repairing torn ligaments and muscles. With demand surging from sports injuries and aging populations, this guide details mechanical evaluation requirements including pullout strength and fatigue testing that manufacturers need for regulatory approval.
When you think about medical implants, knee or hip replacements typically come to mind. However, there are various categories of implants, like those dedicated to repairing bone or soft tissue related conditions. Suture anchors are implants used to repair soft tissue including muscles, ligaments, tendons, and skin.
It is relatively common to hear about a muscle strain or a torn ligament, and these injuries often result in severe pain, coupled with long term implications if untreated. Whether related to athletic events, or general trauma due to falls or injury, surgical assistance is often needed to repair the damage and improve quality of life. Grafts, sutures, bone anchors, and other devices are used to reshape or repair the injury and restore functionality. As a result of the increased occurrences of trauma, bone and suture anchors have been readily accepted in surgical procedures to repair soft tissue injuries.
With an aging population and increased participation in sporting activities, it is expected that the number of soft tissue repair procedures will continue to grow substantially over the next 10 years.
This article will focus on the different methods of suture anchor testing used to evaluate the mechanical performance of design components.
Types of bone and suture anchors
The three most common categories are general suture anchors made of traditional materials (e.g., PEEK), nitinol suture anchors, and absorbable suture anchors. They come in a variety of configurations, such as fully threaded, knotless, or push to lock, and are intended for many applications:
- Upper extremity: rotator cuff, scapholunate, UCL (ulnar collatoral ligament), biceps, and wrist flexor/extensor repairs
- Lower extremity: achilles rupture, foot/ankle instability, quadriceps repairs
Guidance documents
For bone anchor evaluation, there are two main FDA guidance documents that outline the requirements for these devices:
- Premarket Notification (510(k)) Submissions for Bone Anchors
- Class II Special Controls Guidance Document: Surgical Sutures
The guidance documents outline the submissions strategies and outline the recommendations for device description and classification, predicate comparison, biocompatibility, sterility, reprocessing, pyrogenicity, shelf life and packaging, MRI compatibility, non-clinical performance testing, clinical performance testing, and labeling.
There are several published testing methods as well as recommendations outlined in the FDA Guidance, and the method selection depends on the unique design features of the devices. Ultimately, any testing strategy will have to mitigate the observed risks of the device. For example, the fixation, eyelet design and suture must be evaluated. Clinically, common failure modes include loss of fixation in the bone, suture failure through the eyelet or suture failure through the tissue. The interface of the eyelet and the passed-through suture requires additional consideration, particularly as new suture materials are being evaluated.
Sampling
The sterilized device (both bone anchor and suture) should be evaluated in its final packaged condition. There is no minimum accepted sample size, but a sample size of five (5) has been universally accepted per the guidance. Additional samples should be tested dependent on the observed data variability or to mitigate other risk and provide a statistically valid result.
Test methodologies
Dependent on the material of the bone anchor and suture, the relevant test environment should be chosen. For absorbable or nitinol materials, it is recommended to test in saline solution and appropriate temperatures, although other solutions may be used. The FDA Guidance lays out the test methods, but ASTM F564 is commonly also referenced as the methodologies are similar, even though the specification is focused on bone staples.
Suture characterization: The most common method involves testing the tensile strength of the suture. Each specimen is installed into a test fixture, either tied or gripped, looped as recommended by the surgical technique, and pulled to failure at a constant rate. This test quickly evaluates the baseline strength for the suture and intended usage.

Photograph #1: Sample suture tensile pull test setup
Bone anchor insertion testing: The bone anchors are inserted into a bone substitute that has equivalent density to that of the anatomically intended insertion location. The bone substitute should conform to ASTM F1839 - Standard Specification for Rigid Polyurethane Foam for Use as a Standard Material for Testing Orthopaedic Devices and Instruments. A pilot hole may be drilled dependent on the surgical technique, and the bone anchor is then inserted to the intended depth, measuring either torque or force. ASTM F543 which is intended for bone screws is commonly referenced.
Pullout and interconnection testing: This test can replicate three common suture anchor failure modes: the anchor/bone interface, the anchor/suture connection, or the suture itself. Once the bone anchor is inserted into the relevant bone medium per the above method, a constant tensile load is applied to the suture and pulled to failure. This may result in any of the three clinical failure modes and will isolate the weakest component. Additionally, the test method and fixtures can be designed to force failure in either the suture, eyelet/suture interface, or the anchor so that each can be independently evaluated. If the bone anchor consists of an assembly, testing should be performed to evaluate the interconnection mechanisms.

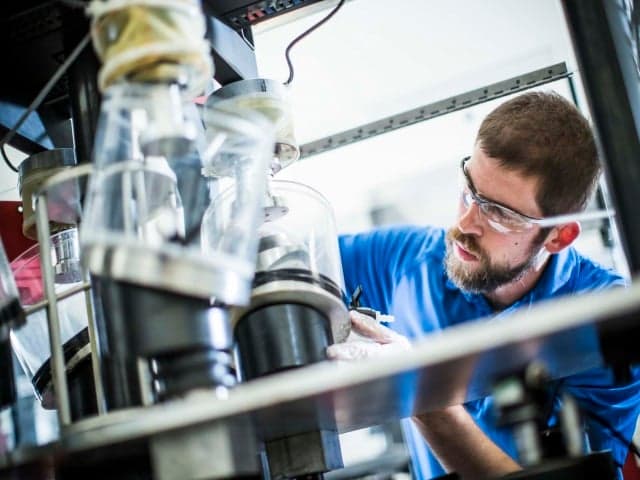
Photograph #2: Sample assembly for pullout and fatigue testing
Fatigue testing: The above test methods evaluate the static strength in the different loading modalities; however, fatigue or cyclic testing should also be performed to evaluate how the device performs over repetitive loading. There are several methods and parameters to consider when performing fatigue testing:
- Predicate performance – first and foremost, the method performed should match the identified predicate test method so that the results can be compared. Bone anchors tend to be more readily available as predicate devices, and it is common
- Number of loops and knotting methods
- Angle of load application – 0°, 45°, and 90° are common angles for evaluation.
- Anchor rotation angle
- Pre-load – the test assembly should be appropriately tensioned to simulate relaxed loading
- Frequencies – as many of the devices are polymeric, test frequencies should not exceed 5 Hz and they are often run slower to minimize fraying effects.
- Test cycles – 500 or 10,000 sinusoidal cycles are a common target cycle count but should be evaluated independently for relevance.
- Loads – loads should be selected to provide adequate comparison.
After completion of the fatigue testing, if suture anchor failure has not occurred before the targeted cycle counts, a static pullout test should be performed to evaluate pre- and post-fatigue results.
Creep testing: For absorbable devices, creep may occur under loading. Testing is performed in the appropriate fluid environment and a static held load is applied to the construct. Displacement should be monitored over the length of time the load is held.
Degradation testing: The FDA Guidance recommends multiple time points for evaluation as degradable materials will lose their structural and mechanical strength overt time. There are several methods for evaluating the levels of degradation:
- ASTM F1635 - Standard Test Method for in vitro Degradation Testing of Hydrolytically Degradable Polymer Resins and Fabricated Forms for Surgical Implants
- ASTM F2502 - Standard Specification and Test Methods for Absorbable Plates and Screws for Internal Fixation Implant
Conclusion
While this overview looks specifically at the test methodologies to evaluate suture bone anchors, many of them can be used in other soft tissue applications. The methods are intended to evaluate the performance of each feature and attempt to replicate suture anchor failure modes. As new developments in the soft tissue repair market are introduced, these suture anchor test methods may be modified and improved, but will continue to serve as the basis for evaluating these types of devices.
For more information about our medical device testing services, contact our experts today.
Related Services

Bone Plate, Bone Screw, and Fixation Device Testing
Our testing service verifies the mechanical integrity of bone plates, screws, and fixation devices through ASTM-standard fatigue, bending, and torsion evaluations, providing critical data for regulatory compliance and trauma reliability.
Foot, Ankle, and Shoulder Replacement Implant Testing
Element offers expert foot, ankle, and shoulder implant testing, covering fatigue, wear, and constraint analysis to support orthopedic device development and regulatory submissions.

Medical Device Testing Services
With Element as your medical device testing partner, you’ll enjoy the benefit of a single comprehensive supplier across feasibility, R&D and prototype trials, through product development, regulatory validation and production quality control.


