Cleanliness and Microbiological Testing
Protect patient safety and accelerate regulatory compliance with our comprehensive cleanliness and microbiological testing. From cleaning validation crucial for biocompatibility to bioburden testing and reprocessing protocols, we deliver end-to-end expertise that maintains device safety while streamlining your path to market approval, all from a single-source supplier.
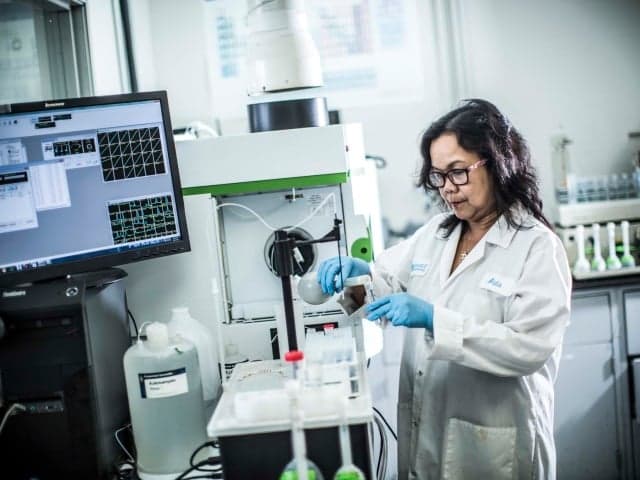
What is Cleanliness and Microbiological Testing at Element?
Cleanliness and Microbiological Testing evaluates cleaning process effectiveness and measures microbial contamination in medical devices. This testing is a critical step for maintaining biocompatibility and controlling the microbiologic profile. At Element, we provide comprehensive testing services to validate cleaning procedures, measure bioburden levels, and verify the removal of physical, chemical, and microbial contaminants for both new and reusable medical devices.

What Can Element Offer You For Cleanliness and Microbiological Testing?
Components and products we test
Components and products we test
Element's testing capabilities cover the full spectrum of medical devices and components throughout their lifecycle. We specialize in:
- Finished medical devices and their components
- Orthopedic implants and surgical instruments
- Raw materials and manufacturing process materials
- Water systems and cleaning agents
- Reusable medical devices requiring reprocessing validation
Key tests offered
Key tests offered
We deliver comprehensive microbiological analysis tailored to your regulatory and quality requirements. Our testing suite includes:
- Bioburden testing - Before final sterilization and packaging, medical devices and pharmaceuticals often need to undergo bioburden testing. This process involves determining the population of viable microorganisms on or inside the product. Bioburden testing applies to non-sterile medical products as well as pre-sterilization evaluations. The results help determine the appropriate sterilization levels and procedures.
- Bacterial endotoxin testing (BET) - BET is essential for the lot release of medical devices and injectable pharmaceutical products. It helps ensure that these products are safe for human use by detecting endotoxins. BET is also part of routine monitoring for water systems and incoming materials, ensuring that production processes do not contribute to contamination.
- Cytotoxicity testing - Cytotoxicity testing is used to assess the toxicity of medical devices and materials. This testing is required for all medical devices before they can receive regulatory approval. It is a quick and standardized process that identifies potentially harmful substances in biomedical materials or devices. The results help screen materials and serve as an initial step in confirming biocompatibility.
- Total Organic Carbon (TOC) testing - TOC testing helps medical device manufacturers monitor water quality to ensure compliance with USP and EP standards. It is also used to validate the cleanliness of both single-use and reusable medical devices. This testing ensures that water systems maintain safe levels of organic compounds and checks for the presence of contaminants or residues from cleaning agents or manufacturing fluids.
- Gravimetric residue analysis - This evaluates the amount of residue extracted from medical device metal components.
Methods and solutions offered
Methods and solutions offered
We employ validated techniques aligned with ISO and USP standards to meet your specific testing needs. Our validated methods include:
Bioburden Testing:
- Microbial Characterization (ISO 11737-1)
Bioburden testing according to ISO 11737 may include testing for aerobic bacteria, spores, fungi, anaerobes, or combinations of these. Typically, the process involves extracting microorganisms from the product, followed by membrane filtration, microbial growth on medium, and counting visible colonies. Alternatively, a plate-count method may be used depending on the product. - Bioburden Recovery Validation (ISO 11135) – Repetitive or Inoculation Method
Bioburden recovery validation is used to develop and validate a product-specific testing procedure. It helps assess the effectiveness of the procedure, evaluate the product’s antimicrobial properties, and establish a recovery factor.
The repetitive (exhaustive) recovery method uses the naturally occurring bioburden to determine how efficiently it can be recovered from the test article.
Whereas the spore inoculation method creates an artificial bioburden to test recovery efficiency.
Bacterial Endotoxin Testing (BET):
- Kinetic Chromogenic & Turbidimetric Methods (USP 85)
This in-vitro quantitative assay detects endotoxins from gram-negative bacteria using Limulus Amebocyte Lysate (LAL) and photometric analysis. It is widely used for medical devices, sterile and non-pyrogenic assemblies, parenteral drugs, and other biological products to predict potential pyrogenic responses.
Validation is required for each device or any changes to processes or materials. Element’s Kinetic Chromogenic method has a detection limit of 0.005 EU/ml, while the Kinetic Turbidimetric method has a detection limit of 0.010 EU/ml.
Cytotoxicity Testing:
- Cytotoxicity (ISO 10993-5, USP 87)
ISO 10993-5 and USP 87 are in-vitro qualitative assays that detect toxins in medical devices, their components, or raw materials, based on their effect on mammalian cell viability.
Testing is done on the final product, representative samples, or materials processed the same way as the final product (see ISO 10993-1). Specimens are prepared according to ISO 10993-12.
If a device or implant is sterilized before use, it should be sterilized according to the manufacturer’s recommendations prior to testing. If non-sterile test samples are used, they must be checked for bacterial contamination to prevent false cytotoxicity results. Testing is performed in triplicate with L929 cells. - Common Testing Methods
The most common cytotoxicity testing method is the MEM Elution method, which simulates actual conditions in which medical devices would be used, often exaggerating these conditions. Other methods used include the Agarose Overlay Method and Direct Contact Method. We also offer cytotoxicity testing for raw materials to help screen your options early in the development process.
Gravimetric residue analysis:
This is conducted using aqueous or organic solvents. While gravimetry alone may not be sensitive enough for thorough cleanliness assessment, it is often combined with additional analytical techniques like FTIR and GC-MS for more accurate results.
Which labs offer this service
Which labs offer this service
Our team operates from Life Sciences hubs across the world, providing global access to our expert capabilities. Find your nearest Life Sciences hub on our Locations Page.
Reprocessing validation expertise
Reprocessing validation expertise
Our specialized validation services support both single-use and reusable devices through comprehensive cleanliness testing. We evaluate cleaning methods against ISO 19227 standards, validate your cleaning processes, and assess cleaning agent residuals through TOC testing. It's important to note that validation approaches differ significantly between production cleaning and reprocessing instructions. Our expertise helps you maintain the highest standards of device cleanliness and safety throughout the product lifecycle. We also offer test failure investigation services to help troubleshoot any issues that may arise.
Standards we test to and components we test
International Standards Organization
- ISO 10993-5
- ISO 10993-12
- ISO 11731-1:2018
- ISO 11135
- ISO 19227
United States Pharmacopeia
- USP <31>
- USP <61>
- USP <62>
- USP <85>
- USP <87>
- USP <161>
- USP <643>
- USP <645>
- USP <1231>
Other Standards
- ANSI/AAMI ST72
- SM 5310C
- ASTM F2459-18
- ASTM F2847-17
- ASTM F3127-16
- ASTM F3208-20
Medical Devices and Components
- Medical devices and their components
- Raw materials
- Orthopedic implants
- Reusable medical instruments
Manufacturing Process Materials
- Water systems
- Cleaning agents
Additional Materials
- Sterile and non-pyrogenic assemblies
- Parenteral drugs
Your Challenges, Our Solutions
Safety validation delivered
Standards compliance achieved
Cleaning effectiveness proven
Reprocessing confidence secured
Why Choose Element

Complete testing solution
Global reach, local service
Regulatory excellence
Fast market access
Related services

Medical Device Testing Services
With Element as your medical device testing partner, you’ll enjoy the benefit of a single comprehensive supplier across feasibility, R&D and prototype trials, through product development, regulatory validation and production quality control.

Medical Device Regulatory Services
Element offers expert medical device regulatory consulting, guiding you through design, risk analysis, and FDA submissions for efficient product approval.

Reusable Medical Device Reprocessing and Testing (GLP Compliant) services
Element's expert validation services for reusable medical devices ensure your equipment is GLP compliant, protecting your staff and your patients.
Chemical Analysis Services
Element’s chemical analysis services provide accurate material verification, compliance testing, and contamination detection. Our advanced methods deliver reliable insights for product development, quality control, and regulatory standards.
